Diabetes biomarkers
Introduction
Diabetes mellitus, or diabetes, is a chronic condition where there is too much glucose in the blood (hyperglycaemia). Glucose is a simple sugar that provides energy for the body. Diabetes is caused by the body not making enough insulin or not effectively using the insulin that it makes to convert glucose to energy. In the short term, high levels of glucose in the blood make you feel tired; the kidneys work hard to pass some of the excess glucose out through the urine which may lead to dehydration and feeling thirsty. If undiagnosed or poorly managed, diabetes can damage blood vessels and nerves and cause long term health complications including heart, kidney, eye and foot damage (WHO 2019, 2023; Diabetes Australia n.d.). The World Health Organization (WHO) describes diabetes or hyperglycaemic disorders by type: Type 1 (insulin dependent), Type 2 (insulin resistant), hybrid diabetes, unclassified diabetes and gestational diabetes (WHO 2019).
The indicators of diabetes that were measured were:
- fasting plasma glucose (FPG)
- glycated haemoglobin (HbA1c).
Self-reported data on diabetes was also collected in other components of the IHMHS. The biomedical results can be used together with the self-reported data to determine diabetes status and estimate disease prevalence rates.
Laboratory test information, including analysis methods and machines used to measure diabetes biomarkers, is available from the Downloads page.
Comparison to other diabetes biomarker data
This is the second time the ABS has collected information on fasting plasma glucose and HbA1c. Information on these biomedical indicators was previously collected in the NHMS 2011–12 and the NATSIHMS 2012–13. For information on time series comparability, see Comparing biomedical collections over time.
FPG, diabetes status and HbA1c data has been collected in other non-ABS surveys. However, caution must be taken when interpreting results due to the differences in scope, definitions, assay and the instrument used, and any thresholds applied in the final analysis.
Fasting plasma glucose (FPG)
Definition
An FPG test measures how much glucose is in the bloodstream at a certain time of day after not eating for eight hours. Plasma glucose is converted into energy in the body by a hormone called insulin. However, people with diabetes do not produce sufficient insulin or do not use the insulin produced effectively to convert plasma glucose into energy. This means that a person with high levels of fasting plasma glucose likely has diabetes (Diabetes Australia n.d.; WHO 2023).
Methodology
FPG results were obtained for persons aged 12 years and over who provided a blood sample and who had fasted for 8 hours or more prior to their blood test.
FPG levels were measured at the Douglass Hanly Moir Pathology (DHM) laboratory using the Hexokinase/G-6-PDH method, using EDTA tubes for blood collection. The FPG test measures the amount of glucose (sugar) circulating in the blood at the time of the test and is expressed as mmol/L.
Cut-off reference values for normal and abnormal results were sourced from WHO guidelines. These guidelines are based on epidemiological data and publications of major clinical trials (WHO 2006, 2019). The cut-off reference values are:
- has diabetes ≥7.0 mmol/L
- at high risk of diabetes 6.1–<7.0 mmol/L
- no diabetes <6.1 mmol/L.
Interpretation
Points to be considered when interpreting data for this topic include the following:
- FPG results do not confirm a specific diagnosis without consultation with a health professional.
- FPG results on their own do not satisfy the definition of diabetes prevalence in the IHMHS. For more information, refer to Diabetes prevalence.
- FPG results cannot distinguish between Type 1 and Type 2 diabetes.
- Impaired glucose tolerance (IGT) and impaired fasting glycaemia (IFG) are intermediate conditions in the transition between normality and diabetes. People with IGT or IFG are at high risk of progressing to Type 2 diabetes, although this is not inevitable.
- Other studies have reported fasting plasma glucose test results using the Oral Glucose Tolerance Test (OGTT). For individuals, the OGTT may be used to confirm diagnosis of diabetes.
- There are several different test methods for measuring FPG, which may produce different results. The data from this topic should therefore be used with caution when comparing fasting plasma glucose results from other studies using a different test method or equation.
Glycated haemoglobin (HbA1c)
Definition
HbA1c is haemoglobin that is bound to a glucose particle in the blood and is a measure of a person’s average blood glucose over the last two to three months. A test result for HbA1c does not indicate blood glucose levels at any one point. An HbA1c test is used to measure the level of control of diabetes in individuals or a population and may also be used to confirm a person has diabetes.
To confirm a diagnosis in asymptomatic individuals, an abnormal HbA1c result should be followed up with repeat testing on a subsequent day, unless two abnormal tests, such as FPG or an OGTT, are already available (WHO 2019; RACGP 2024). HbA1c may lack accuracy in certain cases, where FPG or OGTT can assist diagnosis (RACGP 2024).
Methodology
HbA1c results were obtained for persons aged 12 years and over who provided a blood sample. Fasting was not required for this test.
HbA1c levels were measured at the DHM laboratory using the Sebia Capillary Electrophoresis method. The HbA1c test measures the average blood glucose over the life of a red blood cell. Results are reported as a percentage by the laboratory, and following conversion are expressed as mmol/mol haemoglobin.
Cut-off reference values for HbA1c were taken from WHO Guidelines and are based on epidemiological data and publications of major clinical trials (WHO 2011, 2019). The cut-offs are also referenced in the Australian Evidence-Based Clinical Guidelines for Diabetes (Australian Diabetes Society 2015).
| HbA1c status | HbA1c (%) | HbA1c (mmol/mol haemoglobin) |
|---|---|---|
| Has diabetes | ≥6.5 | ≥48 |
| At high risk of diabetes | 6.0–<6.5 | 42–<48 |
| No diabetes | <6.0 | <42 |
HbA1c units of measurement were reported using both the National Glycohemoglobin Standardization Program (NGSP) units (percentage) and the Système International (SI) units (mmol/mol haemoglobin) as recommended by the International HbA1c Consensus Committee (Hanas et al. 2010).
The equation below was used to convert HbA1c results between the two units, as recommended by the International HbA1c Consensus Committee (Hanas et al. 2010; Jones et al. 2011; Australian Diabetes Society 2015):
\(HbA1c\ (mmol/mol) = 10.93\times HbA1c\ (\%) -23.50\)
In previous ABS biomedical collections, the following equation was used to convert the HbA1c units of measurement reported as a percentage to mmol/mol haemoglobin:
\(HbA1c\ (mmol/mol) = 20 + 11(HbA1c\ (\%)-4)\)
The two equations yield the same answer when rounded to the nearest whole number.
Interpretation
Points to be considered when interpreting data for this topic include the following:
- HbA1c test results do not confirm a specific diagnosis without consultation with a health professional.
- HbA1c results on their own do not satisfy the definition of diabetes prevalence in the IHMHS. For more information, refer to Diabetes prevalence.
- HbA1c results cannot distinguish between Type 1 and Type 2 diabetes.
- Where HbA1c levels indicate a person is at risk of diabetes, prevention interventions might be considered such as lifestyle modifications to achieve HbA1c targets.
- Cut-off reference ranges are based on measuring chronic glycemia periodically as this test may be repeated every 3 or 6 months depending on HbA1c levels and upon consultation with a health professional.
- HbA1c levels are affected by conditions that affect red blood cell survival time or non-enzymatic glycation of haemoglobin (WHO 2011).
- There are several different test methods for measuring HbA1c, which may produce different results. The data from this topic should therefore be used with caution when comparing HbA1c results from other studies using a different test method or equation to convert units of measurement.
Diabetes prevalence
Definition
Diabetes prevalence was derived from IHMHS data using a combination of blood test results and self-reported information on diabetes diagnosis and medication use. Using self-reported information can differentiate between respondents with known diabetes, and those without a prior diagnosis (newly diagnosed diabetes). Three data items are available to users for assessing diabetes status based on different definitions: one for FPG as used in the NHMS 2011–13; one for HbA1c as defined in the 2019 WHO guidelines; and one combining the two test results.
Self-reported diabetes refers to people who reported having ever been told by a doctor or nurse that they had diabetes (including Type 1, Type 2, and type not known) and excludes gestational diabetes. For more information on self-reported diabetes, see the National Health Measures Survey methodology, 2022–24 and National Aboriginal and Torres Strait Islander Health Measures Survey methodology, 2022–24.
The total number of persons with diabetes is defined as the number of persons with known diabetes and newly diagnosed diabetes. Respondents without diabetes were separated into those at high risk of developing diabetes and those with no diabetes. Diabetes status definitions are outlined in the table below.
| Diabetes status | Definition | |
|---|---|---|
| Has diabetes | Known diabetes(a) | A person was considered to have known diabetes if they had ever been told by a doctor or nurse that they have diabetes and:
|
| Newly diagnosed diabetes | A person was considered to have newly diagnosed diabetes if they reported no prior diagnosis of diabetes but had a blood test result greater than or equal to the cut-off for diabetes (≥7.0 mmol/L for FPG, ≥6.5% HbA1c). | |
| Does not have diabetes | At high risk of diabetes | A person was considered at high risk of diabetes if they did not currently have known or newly diagnosed diabetes, but had a blood test result just below the cut-off for diabetes (from 6.1 mmol/L to <7.0 mmol/L for FPG, from 6.1% to <6.5% for HbA1c). |
| No diabetes | A person was considered to not have diabetes if they had a test result below the cut-off for diabetes (≤6.0 mmol/L for FPG, ≤6.0% for HbA1c) and:
| |
a. People who self-reported a diagnosis of diabetes, but reported they were not taking medication and had a test result below the diabetes cut-off were categorised as not having diabetes. These people may be managing the condition with diet and lifestyle interventions.
Methodology
In the NHMS 2011–12 and the NATSIHMS 2012–13, only FPG results were used to determine ‘known’ or ‘newly diagnosed’ diabetes for the purpose of defining and reporting diabetes status. HbA1c was measured and primarily used as an indicator of the success or otherwise of diabetes management over a 3-month period (WHO 2011). Since then, it has been recognised that HbA1c results may be used to diagnose diabetes (WHO 2019; D’Emden et al. 2012; Australian Diabetes Society 2015).
For 2022–24, the ABS has released three different measures of diabetes status, this enables users to utilise which measure best fits their analysis. Caution must be taken to select the appropriate results when comparing the surveys over time.
| Data Item | Methodology |
|---|---|
| Diabetes status (FPG) | Calculated using FPG results to determine known or newly diagnosed diabetes. |
| Diabetes status (HbA1C) | Calculated using HbA1C results to determine known or newly diagnosed diabetes. |
| Diabetes status (combined) | Calculated using either FPG or HbA1C results to determine known or newly diagnosed diabetes. |
Cut-offs for individual FPG and HbA1c data items are described in previous sections. Cut-offs for the combined item are shown in the table below.
| HbA1c (%) | |||
|---|---|---|---|
| FPG (mmol/L) | ≥6.5 | 6.0–<6.5 | <6.0 |
| ≥7.0 | Has diabetes | Has diabetes | Has diabetes |
| 6.1–<7.0 | Has diabetes | At high risk | At high risk |
| <6.1 | Has diabetes | At high risk | No diabetes |
| Did not fast(a) | Has diabetes | Unable to determine | Unable to determine |
a. FPG was not calculated those who did not provide a fasting blood sample. As a result, if a person had a normal HbA1C result (<6.5%) then their combined FPG and HbA1c status is unable to be determined.
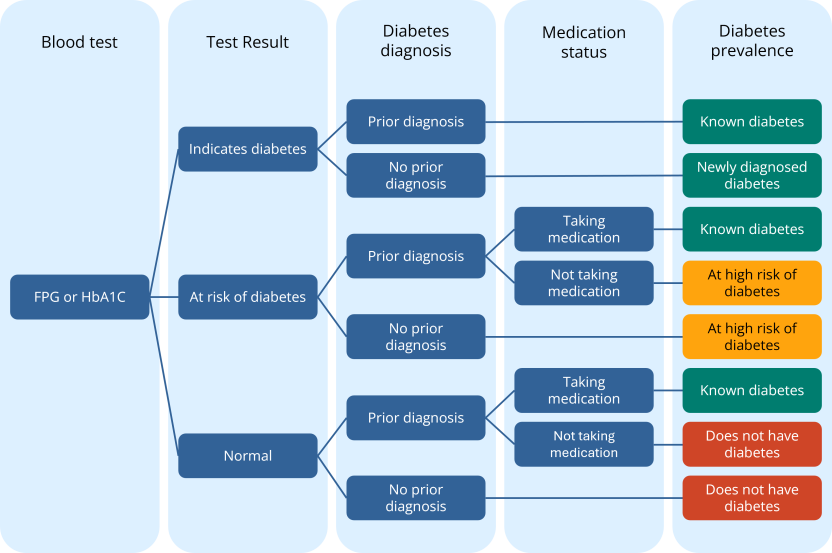
The flowchart below illustrates the determination of diabetes status using test results, self-reported diabetes diagnosis, and medication use.
Determination of diabetes status flowchart
Image
Description
A respondent has diabetes if they have either known diabetes or newly diagnosed diabetes. A respondent has known diabetes if they self-reported a diabetes diagnosis and self-reported taking medications to treat diabetes or if they self-reported a diabetes diagnosis and had a blood test result indicating diabetes. A respondent had newly diagnosed diabetes if the did not self-report a diabetes diagnosis and had a blood test result indicating diabetes.
A respondent does not have diabetes if they are at high risk of diabetes or have no indicators of diabetes. A respondent was at high risk of diabetes if they did not self-report a diabetes diagnosis and had a blood test indicating a high risk of developing diabetes or the self-reported a diabetes diagnosis, did not self-report taking medications for diabetes and had a blood test result indicating a high risk of developing diabetes. A respondent does not have diabetes is they had normal blood test results and did not self-report a diabetes diagnosis or they self-report a diabetes diagnosis, did not self-report taking medications for diabetes and had a blood test result indicating normal levels.
Diabetes management
Definition
In the IHMHS, information is available on diabetes management for those with known diabetes (determined from self-reported diabetes and medication, fasting plasma glucose and/or HbA1c results).
Methodology
HbA1c is the primary measure of how well a person is managing their diabetes. However, there are also other goals for optimum diabetes Type 2 management. The Royal Australian College of General Practitioners (RACGP) lists a number of goals for people with diabetes (RACGP 2024).
| Goal | Advice |
|---|---|
| Diet | Advise individual dietary review. |
| Body Mass Index (kg/m^2) | Advise a goal of 5–10% weight loss for people who are overweight or obese with Type 2 diabetes. |
| Physical activity | Children and adolescents: Aim for at least 60 min/day of moderate to vigorous physical activity, plus muscle- and bone-strengthening activities at least three days per week. Adults: Aim for 150 minutes of aerobic activity, plus two to three sessions of resistance exercise (to a total of ≥60 minutes), per week. |
| Cigarette consumption | Zero per day. |
| Alcohol consumption | No more than 10 standard drinks per week, and no more than four standard drinks on any one day. |
| FPG level | Advise 4–7 mmol/L fasting and 5–10 mmol/L postprandial blood glucose levels. Ongoing self-monitoring of blood glucose is recommended for people with diabetes using insulin, or sulphonylureas. Self-monitoring is also recommended for people with hyperglycaemia arising from intercurrent illness. Routine self-monitoring of blood glucose in patients who are not on insulin should be individualised, depending on the medication they are taking. |
| HbA1c level | Needs individualisation according to patient circumstances. Generally, ≤53 mmol/mol (48–58 mmol/mol) or ≤7% (6.5–7.5%). |
| Lipids |
Initiation of pharmacotherapy is dependent on the assessment of absolute cardiovascular disease risk. This requires using multiple risk factors, which is considered more accurate than the use of individual parameters. Once therapy is initiated, the specified targets apply; however, these targets should be used as a guide to treatment and not as a mandatory target. |
| Blood pressure | ≤140/90 mmHg for general population. <130/80 mmHg for people with diabetes and chronic kidney disease. Treatment targets should be individualised. Lower blood pressure targets may be considered for younger people and for secondary prevention in those at high risk of stroke, if treatment burden does not increase risk. |
| Urine albumin excretion | Urine albumin/creatinine ratio:
|
| Vaccination(a) | Recommended:
Consider:
|
a. Data not collected in the IHMHS
Source: Adapted from RACGP (2024)
Goals for optimum diabetes management for individuals are also provided in the 2020 Australian Evidence-Based Clinical Guidelines for Diabetes (Living Evidence for Diabetes Consortium 2020).
The AUSDRISK Score tool developed in 2010 by the Baker Heart and Diabetes Research Institute on behalf of Australian, State and Territory governments predicts the likelihood of a person having Type 2 diabetes (Department of Health 2010). The information required to complete the tool to derive a score to determine the level of risk of Type 2 diabetes includes:
- age
- sex
- ethnicity
- country of birth
- family history of diabetes (Type 1 or 2)
- diagnosis of high blood glucose, any occasion
- currently taking medication for blood pressure
- smoker status (cigarettes and/or other tobacco products)
- frequency of eating vegetables and fruit (every day/not every day)
- amount of physical activity per week (2.5 hours a week/less than 2.5 hours)
- waist measurement.
References
Australian Diabetes Society (2015, updated 2023), Guidance concerning the use of glycated haemoglobin for the diagnosis of diabetes mellitus, Australian Diabetes Society, accessed 20/02/2025.
Burrow S, Ride K (2016), Review of diabetes among Aboriginal and Torres Strait Islander people, Australian Indigenous HealthInfoNet, accessed 20/02/2025.
Diabetes Australia (n.d.), What is Diabetes, Diabetes Australia website, accessed 20/02/2025.
Department of Health (2010), The Australian type 2 diabetes risk assessment tool (AUSDRISK), Department of Health and Aged Care, accessed 20/02/2025.
d’Emden MC, Shaw JE, Colman PG, Colagiuri S, Twigg SM, Jones GRD, Goodall I, Schneider HG and Cheung NW (2012), The role of HbA1c in the diagnosis of diabetes mellitus in Australia, Medical Journal of Australia, 197(4): 220-221, accessed 20/02/2025.
Hanas R, John G; International HbA1c Consensus Committee (2010), 2010 Consensus Statement on the Worldwide Standardization of the Hemoglobin A1C Measurement, Diabetes Care, 33(8):1903-1904, accessed 20/02/2025.
Jones GR, Barker G, Goodall I, Schneider HG, Shephard MD, Twigg SM (2011), Change of HbA1c reporting to the new SI units, Medical Journal of Australia, 195(1):45–46, accessed 20/02/2025.
Living Evidence for Diabetes Consortium (2020), Australian Evidence-Based Clinical Guidelines for Diabetes, Australian Diabetes Society, accessed 20/02/2025.
Royal Australian College of General Practitioners (RACGP) (2024), Management of type 2 diabetes: A handbook for general practice, RACGP, accessed 20/02/2025.
World Health Organization (WHO) (2006), Definition and diagnosis of diabetes mellitus and intermediate hyperglycaemia, WHO, accessed 20/02/2025.
World Health Organization (WHO) (2011), Use of Glycated Haemoglobin (HbA1c) in the Diagnosis of Diabetes Mellitus, WHO, accessed 20/02/2025.
World Health Organization (WHO) (2019), Classification of diabetes mellitus, WHO, accessed 20/02/2025.
World Health Organization (WHO) (2023), Diabetes, WHO website, accessed 20/02/2025.