Prevalence of mental disorders
The 2007 National Survey of Mental Health and Wellbeing (SMHWB) was designed to provide lifetime prevalence estimates for mental disorders. Respondents were asked about experiences throughout their lifetime. In this survey, 12-month diagnoses were derived based on lifetime diagnosis and the presence of symptoms of that disorder in the 12 months prior to the survey interview. Assessment of mental disorders presented in this publication are based on the definitions and criteria of the World Health Organization's (WHO) International Classification of Diseases, Tenth Revision (ICD-10). Prevalence rates are presented with hierarchy rules applied (ie a person will not meet the criteria for particular disorders because the symptoms are believed to be accounted for by the presence of another disorder). Information on hierarchy rules is provided on the methodology page and within Appendix 1.
In this publication, Tables 1 and 2 provide an overview of the prevalence of mental disorders, with Table 1 focussing on people who had lifetime mental disorders and Table 2 focussing on the subset of people who had 12-month mental disorders.
Of the 16 million Australians aged 16-85 years, almost half (45% or 7.3 million) had a lifetime mental disorder, ie a mental disorder at some point in their life. One in five (20% or 3.2 million) Australians had a 12-month mental disorder. There were also 4.1 million people who had experienced a lifetime mental disorder but did not have symptoms in the 12 months prior to the survey interview.
Image
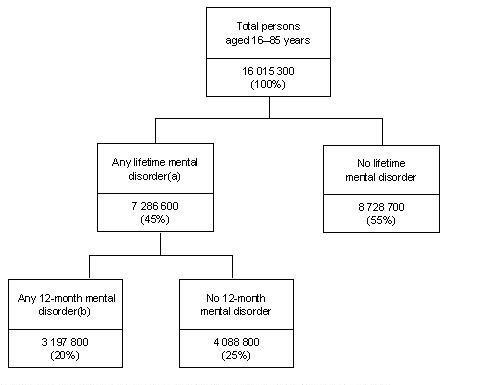
Description
- Person who met criteria for diagnosis of a lifetime mental disorder (with hierarchy)
- Persons who met criteria for diagnosis of a lifetime mental disorder (with hierarchy) and had symptoms in the 12 months prior to interview.
Prevalence of 12-month mental health disorders
Prevalence of mental disorders is the proportion of people in a given population who met the criteria for diagnosis of a mental disorder at a point in time. The diagram below shows the 12-month prevalence rates for each of the major disorder groups (Anxiety, Affective and Substance Use) and prevalence rates for each of the mental disorders within each group.
Image
Description
- Persons who met criteria for diagnosis of a lifetime mental disorder (with hierarchy) and had symptoms in the 12 months prior to interview.
- A person may have had more than one mental disorder. The components when added may therefore not add to the total shown.
- Includes Severe Depressive Episode, Moderate Depressive Episode, and Mild Depressive Episode.
- Includes Harmful Use and Dependence.
There were 3.2 million people who had a 12-month mental disorder. In total, 14.4% (2.3 million) of Australians aged 16-85 years had a 12-month Anxiety disorder, 6.2% (995,900) had a 12-month Affective disorder and 5.1% (819,800) had a 12-month Substance Use disorder.
Women experienced higher rates of 12-month mental disorders than men (22% compared with 18%). Women experienced higher rates than men of Anxiety (18% and 11% respectively) and Affective disorders (7.1% and 5.3% respectively). However, men had twice the rate of Substance Use disorders (7.0% compared with 3.3% for women).
- Persons who met criteria for diagnosis of a lifetime mental disorder (with hierarchy) and had symptoms in the 12 months prior to interview. A person may have had more than one mental disorder.
The prevalence of 12-month mental disorders varies across age groups, with people in younger age groups experiencing higher rates of disorder. More than a quarter (26%) of people aged 16-24 years and a similar proportion (25%) of people aged 25-34 years had a 12-month mental disorder compared with 5.9% of those aged 75-85 years old.
- Persons who met criteria for diagnosis of a lifetime mental disorder (with hierarchy) and had symptoms in the 12 months prior to interview. A person may have had more than one mental disorder.
- Persons who had a 12 month mental disorder as a proportion of all persons in that same age group.
Among all age groups 12-month Anxiety disorders had the highest prevalence, with the highest rate in the 35-44 years age group (18%). People in younger age groups had higher prevalence of 12-month Substance Use disorders (ie the harmful use and/or dependence on alcohol and/or drugs). Of the 2.5 million people aged 16-24 years, 13% (323,500) had a 12-month Substance Use disorder.
- Persons who met criteria for diagnosis of a lifetime mental disorder (with hierarchy) and had symptoms in the 12 months prior to interview. A person may have had more than one mental disorder.
Women aged 16-24 years had nearly twice the prevalence of 12-month Affective disorders compared with men in the same age group (8.4% and 4.3% respectively). Men aged 25-34 years had more than three times the prevalence of 12-month Substance Use disorders compared with women in the same age group (11.3% and 3.3% respectively). Women aged 25-34 years experienced almost twice the prevalence of 12-month Anxiety disorders, compared with men (21% and 12% respectively).
12-month mental disorders
12-month anxiety disorders
Anxiety disorders generally involve feelings of tension, distress or nervousness. A person may avoid, or endure with dread, situations which cause these types of feelings. Anxiety disorders comprise: Panic Disorder, Agoraphobia, Social Phobia, Generalised Anxiety Disorder (GAD), Obsessive-Compulsive Disorder (OCD) and Post-Traumatic Stress Disorder (PTSD). Of people aged 16-85 years, 14.4% (2.3 million) had a 12-month Anxiety disorder. PTSD and Social Phobia were the most prevalent Anxiety disorders (6.4% and 4.7% respectively). Women experienced higher rates of PTSD than men (8.3% compared with 4.6% respectively) and also Social Phobia (5.7% compared with 3.8%).
- Persons who met criteria for diagnosis of a lifetime mental disorder (with hierarchy) and had symptoms in the 12 months prior to interview. A person may have had more than one Anxiety disorder.
12-month affective disorders
Affective disorders involve mood disturbance, or change in affect. Most of these disorders tend to be recurrent and the onset of individual episodes can often be related to stressful events or situations. Affective disorders comprise: Depressive Episode, Dysthymia and Bipolar Affective Disorder. Of people aged 16-85 years, 6.2% (995,900) had a 12-month Affective disorder. Depressive Episode was the most prevalent Affective disorder (4.1%). Women experienced a higher rate of Depressive Episode than men (5.1% compared with 3.1%).
- Persons who met criteria for diagnosis of a lifetime mental disorder (with hierarchy) and had symptoms in the 12 months prior to interview. A person may have had more than one Affective disorder.
- Includes Severe Depressive Episode, Moderate Depressive Episode, and Mild Depressive Episode.
12-month substance use disorders
Substance Use disorders involve the harmful use and/or dependence on alcohol and/or drugs and comprise: Alcohol Harmful Use, Alcohol Dependence and Drug Use disorders. Harmful Use is the pattern of use of alcohol or drugs that is responsible for (or substantially contributes to) physical or psychological harm, including impaired judgement or dysfunctional behaviour. Dependence is a maladaptive pattern of use in which the use of alcohol or drugs takes on a much higher priority for a person than other behaviours that once had greater value. The central characteristic of Dependence is the strong, sometimes overpowering, desire to take the substance despite significant substance-related problems.
Drug Use includes the use of illicit substances and the misuse of prescribed medicines. Four drug categories were included in this survey:
- sedatives, eg serepax, sleeping pills, valium
- stimulants, eg amphetamines, speed
- cannabinoids eg marijuana
- opioids, eg heroin, methadone, opium.
Of people aged 16-85 years, 5.1% (819,800) had a 12-month Substance Use disorder. Alcohol Harmful Use was the most prevalent Substance Use disorder (2.9%). Men experienced higher rates of 12-month Substance Use disorders than women (7.0% and 3.3% respectively). They also had nearly twice the rate of Alcohol Harmful Use (3.8% of men and 2.1% of women).
- Persons who met criteria for diagnosis of a lifetime mental disorder (with hierarchy) and had symptoms in the 12 months prior to interview. A person may have had more than one Substance Use disorder.
- Includes Harmful Use and Dependence.
Population characteristics
Mental health and mental illnesses are determined by multiple and interacting social, psychological, and biological factors, just as they generally are in health and illness (WHO, 2005). Mental health may be impacted by individual or societal factors, including economic disadvantage, poor housing, lack of social support and the level of access to, and use of, health services. A person's socio-economic circumstances (eg employment), may impact on their likelihood of developing a mental disorder. Studies have shown that people of lower socio-economic status have a higher prevalence of mental disorders, particularly Depression, and certain Anxiety disorders (Fryers et al, 2005). Mental illness may also impact on a person's employment, housing, social support, etc. Tables 4 and 5 explore the prevalence of 12-month mental disorders by selected household and population characteristics, including: family composition of household; household income; labour force status; level of highest non-school qualification; country of birth; and marital status.
Living arrangements
Living arrangements give some indication of the level of social support that a person is able to access. People in some living arrangements are more likely to have a mental disorder than others. However, it should be noted that some observed differences may be due to the relationship between living arrangements and age. Of the 745,100 people aged 16-85 years living in a one parent family with children, more than a third (34%) had a 12-month mental disorder. In comparison, 14% of the 4.4 million people living in a couple only households had a 12-month mental disorder.
People living in a one parent family with children had a higher prevalence of Anxiety disorders (26%) than other types of households, while people living in group households were more likely to have a Substance Use disorder (13%).
- Persons who met criteria for diagnosis of a lifetime mental disorder (with hierarchy) and had symptoms in the 12 months prior to interview. A person may have had more than one mental disorder.
Marital status has also been shown to be related to a person's physical and mental health. People who had never been married experienced almost twice the prevalence of 12-month mental disorders compared with people who were married or living in a de facto relationship (28% and 15% respectively). However, this may be partly explained by the number of young people who have never been married, and their higher prevalence of 12-month Substance Use disorders. The prevalence of Substance Use disorders for people who had never been married was more than four times as high as the rate for people who were married or living in a de facto relationship (11.1% compared with 2.5% respectively).
- Persons who met criteria for diagnosis of a lifetime mental disorder (with hierarchy) and had symptoms in the 12 months prior to interview. A person may have had more than one mental disorder.
Labour force status
Education, employment and income are closely related socio-economic characteristics. People with higher educational attainment are more likely to be employed, and of employed people, are more likely to be in a higher skilled occupation (ABS, 2007). Economically disadvantaged people, such as those who are unemployed, are more vulnerable to mental illnesses, as they are more likely to experience insecurity, hopelessness, rapid social change, and risks to their physical health (WHO, 2005). People who have mental illness may also be more likely to fall into economic disadvantage.
A person's ability to sustain themselves and to be a productive member of society, may impact on their mental health and wellbeing. Being unemployed may increase the likelihood of developing mental disorders (Fryers et al, 2005).
Of the 413,600 unemployed people, 29% had a 12-month mental disorder. In comparison, 20% of the 10.4 million people who were employed had a 12-month mental disorder. Unemployed people experienced almost twice the prevalence of Substance Use disorders than employed people (11.1% and 6.0% respectively) and almost three times the prevalence of Affective disorders (15.9% and 5.7% respectively). More than a third of unemployed women (34%) and more than a quarter of unemployed men (26%) had a 12-month mental disorder. Men who were not in the labour force had the lowest prevalence of 12-month mental disorders (14%).
- Persons who met criteria for diagnosis of a lifetime mental disorder (with hierarchy) and had symptoms in the 12 months prior to interview. A person may have had more than one mental disorder.
Life experiences
People may be more or less likely to develop a mental disorder, depending on their life experiences. This survey collected information on a selection of life experiences, including homelessness and incarceration.
Of the 484,400 people who reported ever being homeless, more than half (54%) had a 12-month mental disorder, which is almost three times the prevalence of people who reported they had never been homeless (19%). Of the people who reported ever being homeless, 39% had a 12-month Anxiety disorder, 28% had a 12-month Affective disorder and 18% had a 12-month Substance Use disorder.
- Persons who met criteria for diagnosis of a lifetime mental disorder (with hierarchy) and had symptoms in the 12 months prior to interview. A person may have had more than one mental disorder.
Of the 385,100 people who reported they had ever been incarcerated, 41% had a 12-month mental disorder, which is more than twice the prevalence of people who reported they had never been incarcerated (19%). People who reported they had ever been incarcerated experienced almost five times the prevalence of 12-month Substance Use disorders (23% compared with 4.7%), more than three times the prevalence of 12-month Affective disorders (19% compared with 5.9%), and almost twice the prevalence of 12-month Anxiety disorders (28% compared with 14.1%).
- Persons who met criteria for diagnosis of a lifetime mental disorder (with hierarchy) and had symptoms in the 12 months prior to interview. A person may have had more than one mental disorder.
- Time spent in gaol, prison or a correctional facility.
Contact with family and friends
Interaction with other people is vital to human development. Social relationships and networks can act as protective factors against the onset or recurrence of mental illness and enhance recovery from mental disorders (WHO, 2005). Tables 6 and 7 provide information on the social networks that people have access to and the frequency of contact with their family and friends.
The prevalence of 12-month mental disorders was very similar for people who did and did not have contact with their family. Of the 15.9 million people who had contact with their family, one in five (20%) had a 12-month mental disorder. Of the 121,800 people who had no contact with their family or no family, just under a quarter (23%) had a 12-month mental disorder. However, the prevalence of 12-month mental disorders for people who did and did not have contact with their friends was quite different. Of the 15.7 million people who had contact with their friends, one in five (20%) had a 12-month mental disorder, but for the 352,500 who had no contact with friends or no friends, 38% had a 12-month mental disorder.
Of the people who had contact with their family, those who had family members to rely on or family members to confide in were less likely to have a 12-month mental disorder. One in three people with no family members to rely on (33%) or confide in (33%) had a 12-month mental disorder, compared with around one in six people with three or more family members to rely on (17%) or confide in (15%).
Of the people who had contact with their friends, those who had friends to rely on or friends to confide in were also less likely to have a 12-month mental disorder. Around a quarter (25% and 22% respectively) of the people with no friends to rely on or confide in had a 12-month mental disorder, compared with 18% each for the people with three or more friends to rely on or confide in.
Selected physical and mental health characteristics
Selected health risk factors
Certain health risk factors have an association with mental health problems or mental illness. A number of lifestyle or behavioural factors have been identified as positively and/or negatively impacting on health. These include: level of exercise (physical activity); overweight and obesity; tobacco use (smoking); alcohol consumption; and misuse of drugs (including the use of illicit drugs and/or the misuse of prescribed medicines). Table 8 provides information about each of these selected health risk factors.
Health risks may also be indicated through information about other health and related characteristics, such as the presence of a long-term, or chronic condition. Table 9 provides information on physical conditions, level of psychological distress, suicidal behaviour, disability status, and number of days out of role.
Smoker status
Smoking leads to a wide range of health problems, including cancer and cardiovascular disease. The relationship between smoking and mental illness is complex, as mental illness is also a risk factor for smoking (Access Economics, 2007).
Of the 3.6 million people who identified as current smokers, almost a third (32%) had a 12-month mental disorder. Current smokers had twice the prevalence of 12-month mental disorders compared with people who had never smoked. Of the 8.1 million people who had never smoked, 16% had a 12-month mental disorder.
Current smokers also experienced four times the prevalence of 12-month Substance Use disorders (12%), nearly three times the prevalence of 12-month Affective disorders (12%) and twice the prevalence of 12-month Anxiety disorders (22%) compared with people who had never smoked (3.1%, 4.5%, and 11.1% respectively).
- Persons who met criteria for diagnosis of a lifetime mental disorder (with hierarchy) and had symptoms in the 12 months prior to interview. A person may have more than one mental disorder.
- Daily and other smoker.
Alcohol consumption
Excessive alcohol consumption is a health risk factor that contributes to morbidity and mortality. Alcohol consumption may also interact with mental health in various ways, including:
- people who are diagnosed as having an Alcohol Dependence are more likely to suffer from other mental health problems; and
- people with mental health problems are at particular risk of experiencing problems relating to alcohol (Department of Veteran's Affairs, 2004).
Of the 2.8 million people who reported that they drank nearly every day, more than one in five (21%) had a 12-month mental disorder. Slightly less (18%) of the 6 million people who reported that they drank less than once a month had a 12-month mental disorder.
- Persons who met criteria for diagnosis of a lifetime mental disorder (with hierarchy) and had symptoms in the 12 months prior to interview. A person may have had more than one mental disorder.
- Frequency in the 12 months prior to interview. See Alcohol consumption in the Glossary.
- Includes persons who did not drink in the 12 months prior to interview and those who have never had a drink.
While there were only slight differences in the overall prevalence rates for these two groups, there were significant differences in the prevalence of 12-month Substance Use disorders. People who reported that they drank nearly every day had more than 10 times the prevalence of 12-month Substance Use disorders compared with people who reported that they drank less than once a month (10.5% and 1.0% respectively).
Misuse of drugs
In this survey, the misuse of drugs refers to the use of illicit substances and/or the misuse of prescribed medicines. People must have misused the same drug more than five times in their lifetime before being asked about their use of drugs in the 12 months prior to the survey interview.
Personal and social problems from drug misuse may be substantial and can interfere with personal relationships, employment and psychological health. The misuse of drugs may exacerbate the symptoms of mental illness. For example, Opioid Dependence is often accompanied by high rates of mental disorder, particularly Depression, Social Phobia and other Anxiety disorders. The existence of a mental disorder may also exacerbate drug misuse. For example, people with Anxiety disorders experience high rates of alcohol and drug problems (NCETA, 2004).
Of the 183,900 people who misused drugs nearly every day in the 12 months prior to the survey interview, almost two-thirds (63%) had a 12-month mental disorder. Almost half (49%) of the people who misused drugs nearly every day had a 12-month Substance Use disorder, 38% had a 12-month Anxiety disorder, and 31% had a 12-month Affective disorder.
- Persons who met criteria for diagnosis of a lifetime mental disorder (with hierarchy) and had symptoms in the 12 months prior to interview. A person may have had more than one mental disorder.
- In the 12 months prior to interview. See Misuse of drugs in the Glossary.
- Includes persons who have never used drugs and persons who may have used the same drug less than 5 times in their lifetime.
Level of psychological distress (K10)
The Kessler Psychological Distress Scale (K10) is a widely used indicator, which gives a simple measure of psychological distress. The K10 is based on 10 questions about a person's emotional state during the 30 days prior to the survey interview. Research has found a strong association between high scores on the K10 and the diagnosis of Anxiety and Affective disorders through the current WMH-CIDI (version 3.0). There is also a lesser, but still significant association between the K10 and other mental disorder categories, or the presence of any current mental disorder (Andrews & Slade, 2001).
Of the 409,300 people who had a 'very high' K10 score, 80% had a 12-month mental disorder. More than half (57%) of the 1.1 million people who had a 'high' K10 score also had a 12-month mental disorder. In comparison, there were 11.4 million people who had a 'low' K10 score, of whom, 11% had a 12-month mental disorder.
- Persons who met criteria for diagnosis of a lifetime mental disorder (with hierarchy) and had symptoms in the 12 months prior to interview. A person may have had more than one mental disorder.
- In the 30 days prior to interview. See Psychological distress in the Glossary.
Suicidal behaviour
Suicide is a major public health issue. In this survey, people were asked about suicidal behaviour in their lifetime and in the 12 months prior to the survey interview (refer to Table 9). Of the 368,100 people who reported suicidal ideation in the 12 months prior to the survey interview (that is they had serious thoughts about committing suicide), almost three-quarters (72%) had a 12-month mental disorder.
Disability status
Disability can be described in a number of ways, including: an impairment in body structure or function; a limitation in activities (eg mobility and communication); or a restriction in participation (eg social interaction and work). These different aspects of disability can exist in varying degrees and combinations (AIHW, 2008). Disability status recognises the difficulties that a person may have experienced because of a long-term physical or mental health condition and the limitations, impairments or restrictions to their everyday activities. A long-term health condition, or chronic condition, is a health condition or disorder that has lasted, or is expected to last for six months or more.
This survey assesses the nature and severity of specific activity limitations or restrictions to 'core activities', such as self-care, mobility and communication, and in schooling or employment, for people who reported they have a chronic condition. Disability status is calculated based on responses to questions from the standard ABS Short Disability Module. Responses are combined to create a scale measure which ranges from 'mild' to 'profound' core-activity limitation and also assesses whether there is a schooling and/or employment restriction. A profound or severe core-activity limitation means that the respondent always or sometimes needed personal assistance or supervision with their daily activities.
Of the 481,700 people who had a profound or severe core-activity limitation, 43% had a 12-month mental disorder. People who had a profound or severe core-activity limitation had almost three times the prevalence of 12-month Anxiety disorders (33%) and five times the prevalence (20%) of 12-month Affective disorders compared with people who had no disability or no specific limitations or restrictions (11.6% and 4.2% respectively).
- Persons who met criteria for diagnosis of a lifetime mental disorder (with hierarchy) and had symptoms in the 12 months prior to interview. A person may have more than one mental disorder.
- Core-activity limitation. See Disability status in the Glossary.
Comorbidity
Comorbidity is the co-occurrence of more than one disease and/or disorder in an individual. Mental disorders may co-occur for a variety of reasons, and Substance Use disorders frequently co-occur (CDHAC, 2001). A person with co-occurring diseases or disorders is likely to experience more severe and chronic medical, social and emotional problems than if they had a single disease or disorder. People with comorbid conditions are also more vulnerable to alcohol and drug relapses, and relapse of mental health problems. Higher numbers of disorders are associated with greater impairment, higher risk of suicidal behaviour and greater use of health services.
In this publication, information is presented on both the comorbidity of mental disorder groups and physical conditions (Table 10), and the co-occurrence of more than one mental disorder with physical conditions (Table 11). As people with comorbid disorders generally require higher levels of support than people with only one disorder, Table 13 presents the number of 12-month mental disorders by services used for mental health problems.
All comorbidity tables in this publication are presented without the WMH-CIDI 3.0 hierarchy rules applied. Presenting the 12-month mental disorders without hierarchy provides a more complete picture of the combinations of symptoms and disorders experienced by individuals. For more information on hierarchy rules see the methodology and Appendix 1.
Image
Description
- Persons who met criteria for diagnosis of a lifetime mental disorder (without hierarchy) and had symptoms in the 12 months prior to interview
- A physical condition that a person had or received treatment for in the 12 months prior to interview. See Physical condition in the Glossary
- These categories are mutually exclusive.
Comorbidity of mental disorders and physical conditions
Of the 16 million Australians aged 16-85 years, almost three in five (58%) had a 12-month mental disorder or physical condition: 8.2% (1.3 million) had mental disorders only and 11.7% (1.9 million) had both a mental disorder and a physical condition. The most common comorbidity was a combination of 12-month Anxiety disorders and physical conditions (6.0%).
Comorbidity of mental disorders
There were 1.4 million (8.5%) people who had two or more 12-month mental disorders. Of Australians aged 16-85 years, 3.4% (548,100) had disorders from the same group (eg two Anxiety disorders) and 5.1% (812,300) had disorders from different groups (eg one Anxiety disorder and one Affective disorder).
Services used for mental health problems
Information on services used for mental health problems supports the development of policies and programs to assist people with mental disorders. Monitoring mental health and mental illness within populations, both currently and over time, also provides information on the level and type of interventions that may be needed.
This survey collected information on services used by respondents for mental health problems in their lifetime and in the 12 months prior to the survey interview. The types of services used varied and included: professional treatment of physical and emotional problems, such as visits to a general practitioner or psychologist; hospital admissions; and self-management strategies, such as using the Internet or going to a self-help group. Tables 12 and 13 provide information on professional consultations for mental health problems, focussing on the 12 months prior to the survey interview.
Of Australians aged 16-85 years, 12% (1.9 million) accessed services for mental health problems in the 12 months prior to the survey interview. Of these, three in five (59%) people had a 12-month mental disorder, and one in five either met the criteria for lifetime diagnosis of a mental disorder but did not have symptoms in the 12 months prior to the survey interview (20%) or had no lifetime mental disorder (21%). People who were not diagnosed with a lifetime disorder may have consulted a health professional for a mental disorder that was not included in this survey or for some other type of mental health problem.
Of the 3.2 million people with a 12-month mental disorder, more than a third (35%) accessed services for mental health problems. Women with a 12-month mental disorder accessed services for mental health problems more than men (41% compared with 28%). Almost one in three (30%) women with a 12-month mental disorder visited a general practitioner, compared with just over one in six (18%) men. Women were also more likely to visit some other type of health professional, such as a complementary or alternative therapist, compared with men (8.0% and 4.7% respectively).
- Persons who met criteria for diagnosis of a lifetime mental disorder (with hierarchy) and had symptoms in the 12 months prior to interview. A person may have more than one mental disorder.
- In the 12 months prior to interview. See Services used for mental health problems in the Glossary.
- Includes mental health nurse and other professionals providing specialist mental health services.
- Includes medical specialist, other general specialist, complementary and alternative therapist.
- A person may have used more than one service for mental health. The components when added may therefore not add to the total shown. Also includes hospital admissions.
Service use and comorbidity
People with comorbid disorders had greater use of health services. Table 13 in this publication presents the number of 12-month mental disorders without hierarchy and services used for mental health problems. People with one disorder only were less likely to use services for their mental health than those with two or more disorders (23% and 52% respectively). Of the 1.8 million people with one disorder only, those with a 12-month Affective disorder were much more likely to use health services, than those with an Anxiety or Substance Use disorder. Of the people who had a 12-month Affective disorder only, 45% used services for their mental health, with most of these (80%) seeing a General Medical Practitioner (GP).
People with two or more mental disorders (1.4 million) had a rate of service use more than twice that of people with one disorder only (52% and 23% respectively). People with two or more disorders from different groups had a higher rate of service use than people with two or more disorders from the same group (57% and 43% respectively). Again, people were more likely to see a GP than other types of health professional: 43% of people with two or more disorders from different groups and 35% of people with two or more disorders from the same group saw a GP. Almost a quarter (24%) of people with two or more disorders from different groups saw a Psychologist for their mental health.
- Persons who met criteria for diagnosis of a lifetime mental disorder (without hierarchy) and had symptoms in the 12 months prior to interview.
- These categories are mutually exclusive.
Perceived need for help
Whether people had a perceived need for help was assessed in relation to: information, medication, counselling, social intervention, and skills training. Table 14 presents information on perceived needs for people who used services for mental health problems, and whether or not they had a 12-month mental disorder. Table 15 focuses on people who had a 12-month mental disorder who did not use services for mental health problems.
Perceived need for help for people who used services
Of people with a 12-month mental disorder who used services, just over a quarter (26%) did not have their need for counselling met or only had their need partially met. A slightly higher proportion, 29% did not have their need for information met or only had their need partially met.
- Persons who met criteria for diagnosis of a lifetime mental disorder (with hierarchy) and had symptoms in the 12 months prior to interview. A person may have more than one mental disorder.
- In the 12 months prior to interview. See Services used for mental health problems in the Glossary.
- Need partially met and need not met.
- Includes help to sort out practical issues, such as money or housing, or help to meet people for support or company.
- Includes help to improve ability to work, to care for self, or to use time effectively.
Perceived need for help for people who did not use services
There were 2.1 million people with a 12-month mental disorder who did not use services for mental health problems. Of those who did not use services for mental health problems, 10% perceived that their need for counselling was not met.
- Persons who met criteria for diagnosis of a lifetime mental disorder (with hierarchy) and had symptoms in the 12 months prior to interview. A person may have more than one mental disorder.
- In the 12 months prior to interview. See Services used for mental health problems in the Glossary.
- Includes help to sort out practical issues, such as money or housing, or help to meet people for support or company.
- Includes help to improve ability to work, to care for self, or to use time effectively.
End notes
Access Economics, 2007. Smoking and mental illness: Costs. A report for SANE Australia. Retrieved 18 August 2008 from http://www.accesseconomics.com.au/
Andrews, G and Slade, T, 2001. Interpreting scores on the Kessler Psychological Distress Scale (K–10) in the Australian and New Zealand Journal of Public Health, vol. 25, no. 6, pp494-497. Retrieved 18 June 2008 from Informit database.
Australian Bureau of Statistics (ABS), 2007. Education and Work, Australia, 2007 (cat. no. 6227.0). Canberra.
Australian Bureau of Statistics (ABS), 2006. National Health Survey: Summary of Results, 2004-05 (cat. no. 4364.0). Canberra.
Australian Health Ministers, July 2003. National Mental Health Plan 2003-2008. Retrieved 12 June 2008 from http://www.health.gov.au/
Australian Institute of Health and Welfare (AIHW), 2008. Australia's Health, 2008 (cat. no. AUS99). AIHW, Canberra.
Commonwealth Department of Health and Aged Care (CDHAC), 2001. National Comorbidity Project. A report on the National Comorbidity Workshop prepared by M Teesson and L Burns (eds) of the National Drug and Alcohol Research Centre. Commonwealth of Australia, Canberra.
Department of Health and Ageing (DoHA), 2007. National Mental Health Report, 2007: Summary of Twelve Years of Reform in Australia's Mental Health Services under the National Mental Health Strategy 1993-2005. Commonwealth of Australia, Canberra.
Department of Veteran's Affairs (DVA), 2004. Alcohol and mental health. Retrieved 10 September 2008 from http://www.therightmix.gov.au/
Fryers, T, Melzer, D, Jenkins, R, and Brugha, T, 2005. The distribution of the common mental disorders: Social inequalities in Europe in Clinical Practice and Epidemiology in Mental Health (online), vol. 1, no. 14. Retrieved 15 August 2008 from BioMed Central http://www.pubmedcentral.nih.gov/
Kessler, RC, and Ustan, TB, 2004. The World Mental Health (WMH) Survey Initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) in the International Journal of Methods in Psychiatric Research, vol. 13, no. 2, pp93-121. Retrieved 2 July 2008 from http://www.hcp.med.harvard.edu/wmhcidi/
National Centre for Education and Training on Addiction (NCETA) Consortium, 2004. Alcohol and Other Drugs: A handbook for health professionals. Retrieved 11 September 2008 from http://www.aodgp.gov.au
World Health Organization (WHO), 2007. International Classification of Diseases and Related Health Problems, 10th Revision (ICD-10 online). Retrieved 19 June 2008 from http://www.who.int/
World Health Organization (WHO), 2005. Promoting mental health: Concepts, emerging evidence, practice. A report of the WHO, Department of Mental Health and Substance Abuse in collaboration with the Victorian Health Promotion Foundation and the University of Melbourne by Herman, Saxena, and Moodie (eds). Retrieved 28 August 2008 from http://www.who.int/
World Health Organization (WHO), 2001. The World Health Report 2001- Mental health: New understanding, New hope. Retrieved 12 June 2008 from http://www.who.int/