This publication contains preliminary death counts by date of occurrence for Australia.
This series was introduced in June 2020 in response to the COVID-19 pandemic in Australia. The report provides an early indication of the pattern of mortality. There are many factors that may influence counts of deaths on a week to week basis, so deviations from baseline counts for individual weeks should be treated with caution.
The results for all past publications can be accessed by selecting ‘View all releases’ in the header of this publication.
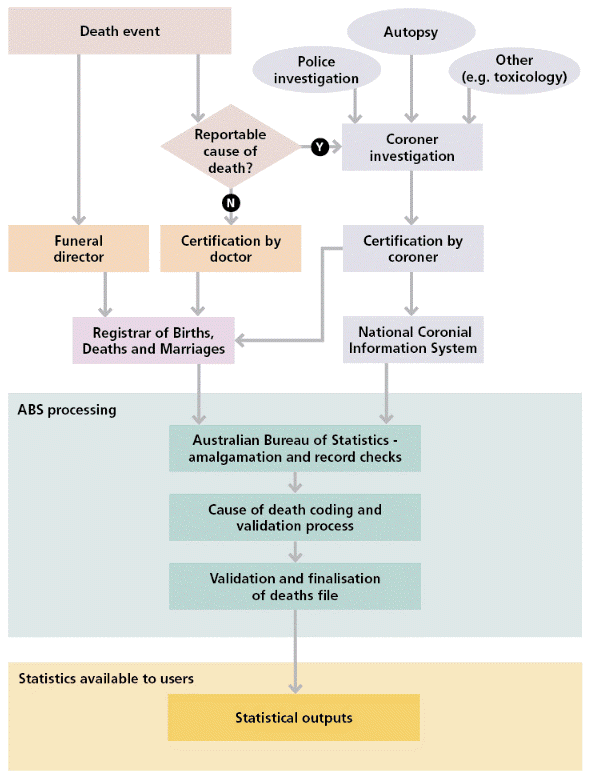
Complete analysis of mortality data is only possible when all death records (both coroner and doctor) are received and processed. Death counts in this report will not be comparable with those reported in Deaths, Australia or Causes of Death, Australia. Differences are explained in more detail throughout the methodology. Death counts in this report may also not be comparable with other data sources based on the provisional data. Until it has been finalised, the data is subject to continuous quality improvement.
For more complete analysis of 2020 and 2021 mortality statistics, please refer to the Deaths and Causes of Death reports linked above.